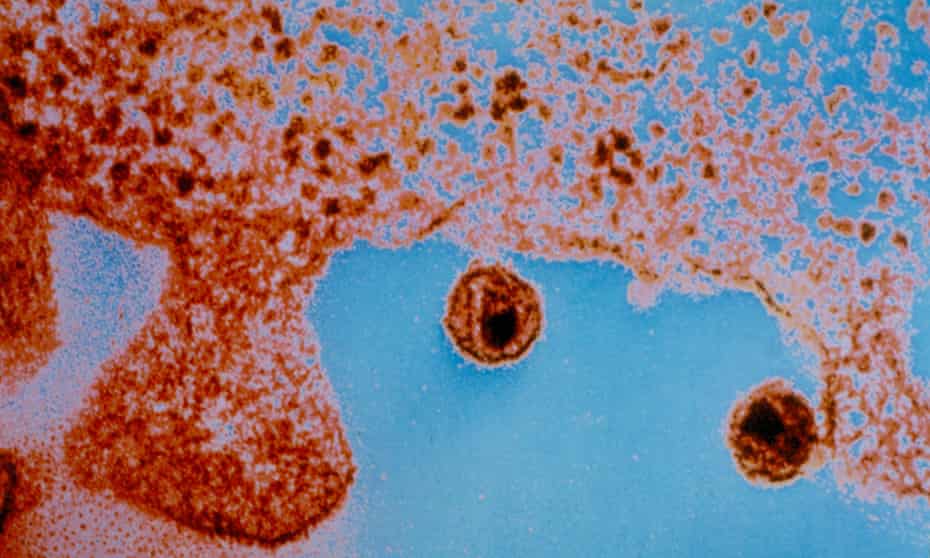
According to studies conducted in Denver, Colorado, scientists appear to have cured a third individual, and the first woman, of HIV using a unique stem cell transplant method.
According to the reports, a lady of mixed race was treated using a new approach that utilised umbilical cord blood, which is more easily available than adult stem cells, commonly used in bone marrow transplants.
Umbilical cord stem cells do not have to be as tightly matched to the recipient as bone marrow cells.
“We estimate that there are approximately 50 patients per year in the US who could benefit from this procedure,” said Dr Koen van Besien, one of the doctors involved in the treatment.
“The ability to use partially matched umbilical cord blood grafts greatly increases the likelihood of finding suitable donors for such patients.”
The researchers gave some case details at the Conference on Retroviruses and Opportunistic Infections in Denver. Scientists have dubbed the woman the “New York patient” since she had her therapy at the New York-Presbyterian Weill Cornell Medical Center.

She was diagnosed with HIV in 2013. She was diagnosed with leukaemia four years later. To cure her cancer, she received cord blood from a partially matched donor in a process called a haplo-cord transplant. A close relative also donated blood to help her immune system while she was undergoing the operation.
Patients are given extra adult stem cells following an umbilical cord blood transplant. The stem cells proliferate swiftly but are eventually replaced by other cells.
Although cord blood stem cells are more flexible than adult stem cells, they do not produce enough to be effective in cancer therapies in adults. As a result, with haplo-cord transplants, the extra stem cell transplant helps compensate for the lack of cord blood cells.
“The role of the adult donor cells is to hasten the early engraftment process and render the transplant easier and safer,” said Van Besien.
Since her transplant in August 2017, the woman has been remission from leukaemia for almost four years. In addition, three years after the transplant, her physicians stopped her HIV medication. As a result, she hasn’t had any recurrences of the infection in fourteen months.
According to the researchers, most donors in registries are of Caucasian background. As a result, allowing for just partial matches may enable the treatment of patients who have both HIV and cancer and those from more mixed ethnic origins.
“The fact that she’s mixed race, and that she’s a woman, that is really important scientifically and really important in terms of the community impact,” Dr Steven Deeks, an Aids expert at the University of California, said.
Although women account for more than half of the world’s 35 million HIV infections, they account for just 11% of participants in cure studies.

Despite knowing that Deeks was not engaged in the case, he admitted that “these are stories of providing inspiration to the field and perhaps the road map.”
“Umbilical stem cells are attractive,” he added. “There’s something magical about these cells and something magical perhaps about the cord blood in general that provides an extra benefit.”