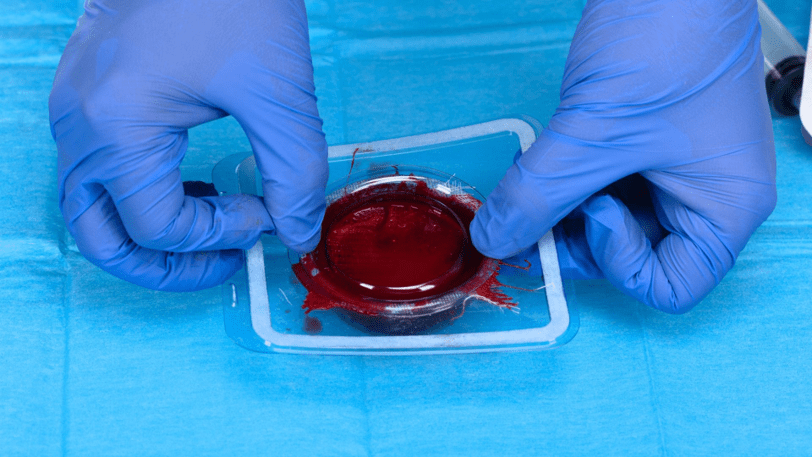
When chronic wounds hinder the natural healing process by preventing blood platelets from reaching the affected areas, traditional methods like bandages and specialized dressings may fall short. However, RedDress, a US-based medical device company, has introduced a groundbreaking solution to this problem. Their proprietary blood-based technology utilizes a patient’s own blood to create real-time external blood clots, jump-starting the healing process.
In an interview with Interesting Engineering, RedDress’ CEO and Co-founder, Alon Kushnir, sheds light on how this innovation is revolutionizing chronic wound management. Kushnir explains that blood clots, though often viewed negatively, play a crucial role in the body’s natural healing process. RedDress’ technology recreates this process for patients who struggle to heal their own wounds, such as those with diabetic ulcers or venous ulcers. The procedure, which can be performed at the point of care in about 20 minutes, involves using the patient’s own whole blood to create an all-fibrin clot that contains the necessary cells for wound healing.
This approach has shown remarkable success, with a 72 percent rate of complete wound closure at the 12-week mark compared to the standard method of care, which achieves only a 22 percent closure rate.
The effectiveness of RedDress’ technology was demonstrated through a pilot study conducted on patients with chronic neuropathic diabetic foot ulcers. The study participants received multiple applications of the blood clot product over a period of 12 weeks, leading to significant wound healing. These positive outcomes highlight the potential of this innovative solution in effectively treating chronic wounds.
The journey of developing this technology began with the idea of treating burns using blood clots from donated blood. However, the focus shifted to treating chronic wounds related to diabetes due to the potential for greater impact. ActiGraft, the name given to this technology, received FDA clearance and the CE mark in 2020, enabling its use in various types of wounds.

RedDress continues to explore new ideas and expand its product line. They are currently conducting clinical trials for treating anal fistula in Crohn’s and inflammatory bowel disease patients, with promising results. The company’s research also extends to nerve healing, with ongoing pre-clinical trials focused on creating nerve cells where needed.
While ActiGraft has already made a significant impact in the field of wound care, RedDress is committed to further research and development. They aim to address challenging wounds that have limited treatment options, such as fistulas, pilonidal cysts, and stomas.
As Kushnir emphasizes, the team at RedDress is driven by the vision of regenerative medicine as the future of the human healing process. Their innovative blood-based technology and ongoing research efforts are paving the way for a new era in wound management and regenerative medicine.
Overall, RedDress’ ActiGraft offers a promising solution for patients with chronic wounds, revolutionizing the treatment landscape and bringing hope to those who face limited options for healing.