Heart attacks cause the formation of non-beating scar tissue on the affected area of the organ and this leads to heart failure. However, the risk can be minimized with the help of an implanted device which would deliver medication directly to the affected tissue.
After a heart attack occurs, non-beating scar tissue forms on the part of the organ that was affected and this can lead to heart failure. There could be new hope, however, in the form of an implanted device that delivers medication directly to that tissue. Heart-healing medication is generally directed to the body as a whole, or it’s injected into the heart directly.
In order to minimize side effects elsewhere in the body, the doses of the medication need to be kept fairly low, while administering it into the body as a whole. As a consequence, rather small amounts of the medication actually reach the heart. In the case of injecting it directly into the heart, the process requires several injections to the heart, involving multiple surgeries to access the organ.
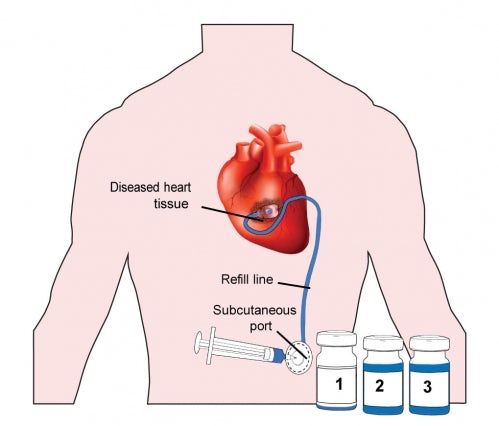
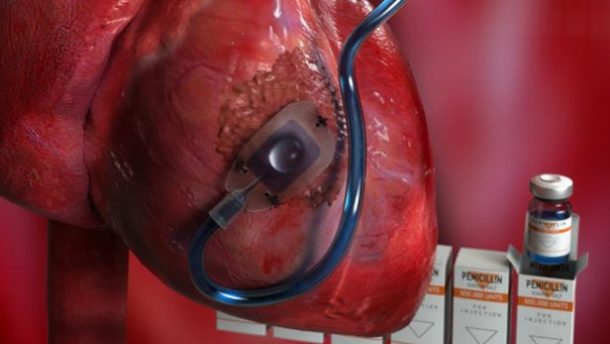
The revolutionary Therepi device diminishes the risks associated with both the processes. The device is created by a team of American and Irish scientists; it’s made of a thin flexible tube with a small polymer reservoir at the end. That reservoir, which is semi-spherical with a flat underside, gets sutured to the scar tissue on the heart. The tube is routed up to an opening in the patient’s skin.
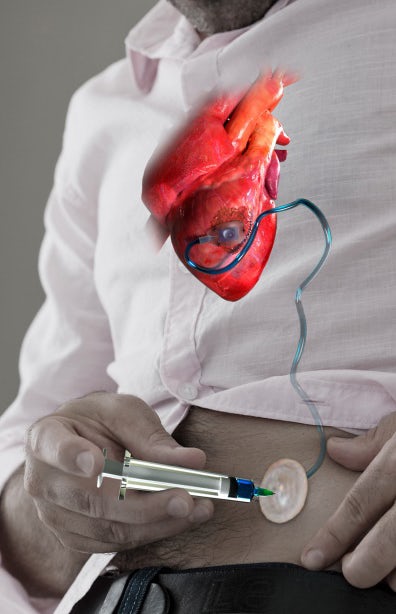
Through the skin port, which travels down the tube into the reservoir, multiple doses of medication can be manually pumped one after the other. The medication is released straight into the tissue, gradually, through the reservoir as the underside of that reservoir is made of a sponge-like, permeable polycarbonate membrane.
In one month progress during lab testing, Therepi was successful in delivering stem cell-based medication to the scarred hearts of rats.
“The stem cells remain in the reservoir and act as production factories, constantly releasing factors that are transported out of the device and modulate healing,” says MIT assistant professor Ellen Roche. “With multiple replenishments, the ‘dose’ of these factors is increased, as is their potential to elicit a functional benefit. At 28 days, we observed, among other cardiac parameters, an increased ejection fraction, meaning the percentage of blood ejected compared to total volume of chamber increased.”
In comparison, the heart which received a single dose of stem cells or received no treatment at all had a little difference. It is expected, delivering medications directly to organs, other than the human heart can be made possible through Therepi. Moreover, a biodegradable version is also in the making, through which, patients would not require going into a second surgery for the removal of the device.
This new Therepi device will definitely save many lives.