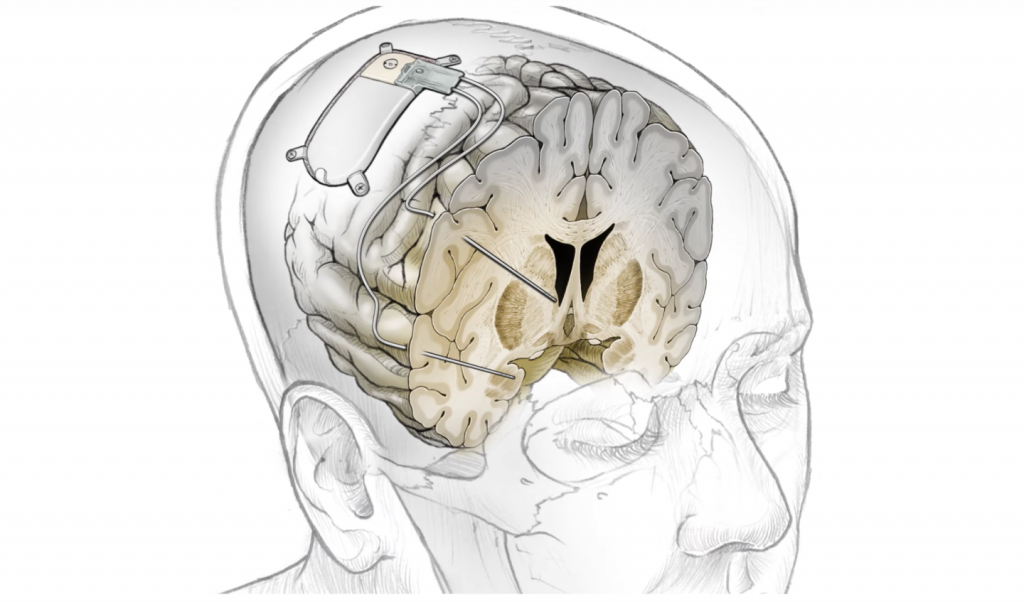
A brain implant, according to a groundbreaking study, can relieve severe depression by electrically stimulating certain brain regions. The experimental implant detects biomarkers that identify depression and whacks a key brain region to break the loop and ease depressive symptoms.
“This study points the way to a new paradigm that is desperately needed in psychiatry,” explains Andrew Krystal, the study’s co-senior author. “We’ve developed a precision-medicine approach that has successfully managed our patient’s treatment-resistant depression by identifying and modulating the circuit in her brain that’s uniquely associated with her symptoms.”
Researchers at the University of California, San Francisco, implanted temporary thin wire electrodes into Sarah’s brain, the first human patient to be treated with the experimental brain implant. 36-year-old Sarah had been suffering from persistent depression for years. She felt suicidal multiple times. Nothing she’d done, including electroconvulsive therapy, had worked.

“I was at the end of the line,” she explains. “I was severely depressed. I could not see myself continuing if this was all I’d be able to do if I could never move beyond this. It was not a life worth living.”
A previous study attempted to establish a relationship between specific moods and electrical brain activity changes. While some researchers concentrated on brain areas that were treated with electrical jolts and improved depressive symptoms.
However, “This new study puts nearly all the critical findings of our previous research together into one complete treatment aimed at alleviating depression,” says co-senior author Edward Chang.
First, the researchers extensively monitored Sarah’s brain’s electrical activity for 10 days to detect specific patterns linked with depressive symptoms. The researchers concentrated their efforts on a particular region of the amygdala that emerged with activity regularly, signalling the start of acute depressive symptoms. They also established that a small burst of electricity to another region of her brain, called the ventral striatum, significantly improved these symptoms. Next, they implanted a neurostimulation device and set it up to trigger a tiny pulse of electricity in that area when it detects high levels of activity associated with depression symptoms.

“In the early few months, the lessening of the depression was so abrupt, and I wasn’t sure if it would last,” Sarah says. “But it has lasted.”
Before the device was implanted, Sarah had a score of 36 out of 54 on the Montgomery-Åsberg Depression Rating Scale; a scoring system often used to rate the severity of these symptoms. After two weeks, her score fell to 14. Now it is under 10.
“The idea of stimulating somebody and just a few seconds later, them saying, ‘My depression is gone’ … it is just stunning,” Krystal said to StatNews. “They have this experience where they haven’t felt this good in years, they get hope. They feel like there’s a sense of relief that it feels like it’s not their fault because it’s changeable by modulating brain circuitry.”
This study is “interesting,” according to Jonathan Roiser, a neurologist at University College London, although he emphasises that it only involves one patient. However, it’s unclear how a system like this will work in other situations.
“Although this kind of highly invasive surgical procedure would only ever be used in the most severe patients with intractable symptoms, it is an exciting step forward due to the bespoke nature of the stimulation,” says Roiser. “It is likely that if trialled in other patients, different recording and stimulation sites would be required, as the precise brain circuitry underlying symptoms probably varies between individuals.”
According to The study’s author, Katherine Scangos, further research is necessary before using this therapy in an actual clinical context.
“We need to look at how these circuits vary across patients and repeat this work multiple times,” says Scangos. “And we need to see whether an individual’s biomarker or brain circuit changes over time as the treatment continues.”
The researchers have enlisted two more volunteers for this study. The ultimate goal is to enrol 12 participants, and the current study will go until 2035.
The new study was published in the journal Nature Medicine.
Here’s a look at the breakthrough treatment from the UC San Francisco team:
Source: UCSF