A protein implant made from pig skin may be able to give blind patients their vision back, claims new research. According to research, nobody who underwent the operation was still blind two years later. In addition, three people who were previously blind also had 20:20 vision after the ground-breaking procedure.
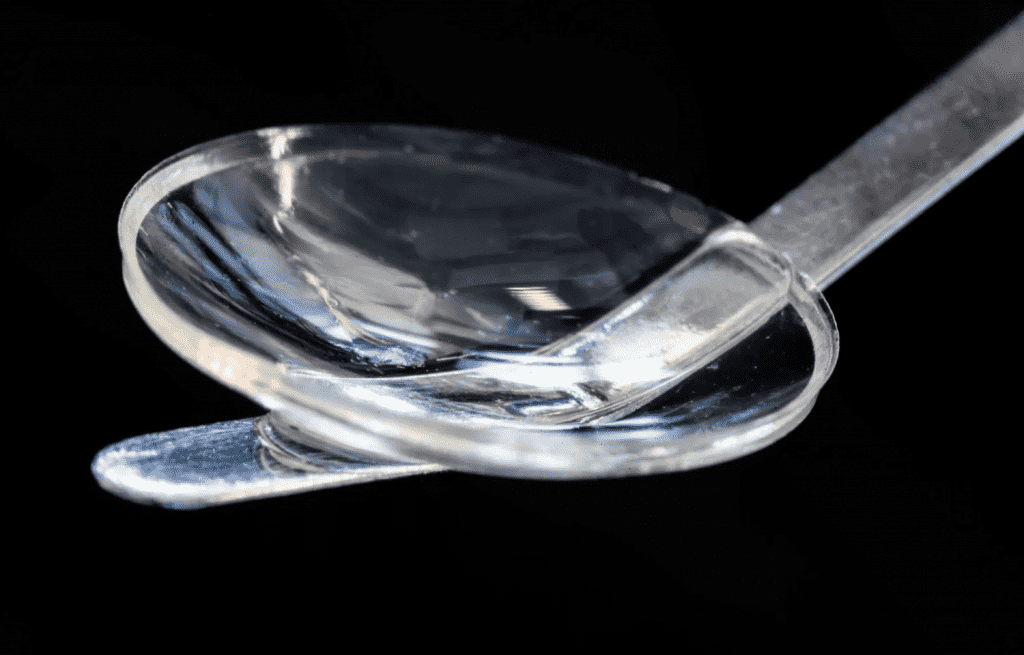
The implant, comprised of pig skin collagen protein, resembles the cornea, the outermost transparent layer of the human eye.
Corneal injury or illness causes blindness in more than 12 million individuals worldwide. Typically, these patients’ vision can only be recovered through a human cornea transplant from a donor. Unfortunately, only one out of every 70 patients who require a corneal transplant gets one.

According to the researchers, this new transplant is mass-producible and has a two-year shelf life, whereas donated human corneas must reach patients within two weeks. The new method could benefit people in poor countries where human corneal transplants are particularly scarce.
A Swedish team recruited 14 blind people and six partially sighted people in India and Iran for the study. Keratoconus is a disorder in which the cornea gets so thin that it can lead to blindness.
The researchers discovered that none of the 14 participants who were blind before the operation were still blind after that. Three of the blind Indian subjects received excellent vision after the transplant. There were no difficulties observed during the process or after a two-year follow-up.
An eight-week course of eye drops was all that was required to keep a patient’s eye from rejecting the implant. Traditional corneal transplants can require several years of treatment before full recovery.
The trial’s primary goal was to determine whether the implant was safe to use. The transplant’s effectiveness, according to the team, was astounding. The team employed collagen molecules derived from pig skin that were extensively purified and synthesized under rigorous human-use conditions to create it. Since the pig skin is not the same as that used in the meat sector, it is easy to get and economically advantageous.
When the implant was built, the researchers fixed the free collagen molecules to create a solid and clear material that could endure handling and implantation in the eye. However, a larger clinical trial must be conducted before scientists can deem it safe and successful enough to be used in hospitals.
“The results show that it is possible to develop a biomaterial that meets all the criteria for being used as human implants, which can be mass-produced and stored for up to two years and thereby reach even more people with vision problems. Furthermore, this gets us around the problem of shortage of donated corneal tissue and access to other treatments for eye diseases,” says Professor Neil Lagali from Linköping University in a media release.
“Safety and effectiveness of the bioengineered implants have been the core of our work,” says Dr Mehrdad Rafat from LinkoCare Life Sciences AB, who designed and developed the implant.
“We’ve made significant efforts to ensure that our invention will be widely available and affordable by all and not just by the wealthy. That’s why this technology can be used in all parts of the world.”
In addition, the team has created a new, minimally invasive way of treating keratoconus. A keratoconus patient’s cornea is surgically removed and replaced with a donor cornea, which physicians sew into place with stitches. This type of surgery is invasive and is only performed at larger hospitals. Stitches are no longer required with this innovative surgical technique.
The corneal incision can be done precisely with a sophisticated laser or by hand with a simple surgical instrument. The procedure was first conducted on pigs and was discovered simpler and perhaps safer than a traditional cornea transplant.
“A less invasive method could be used in more hospitals, thereby helping more people. With our method, the surgeon doesn’t need to remove the patient’s tissue. Instead, a small incision is made, through which the implant is inserted into the existing cornea,” says Lagali.
The findings are published in the journal Nature Biotechnology.