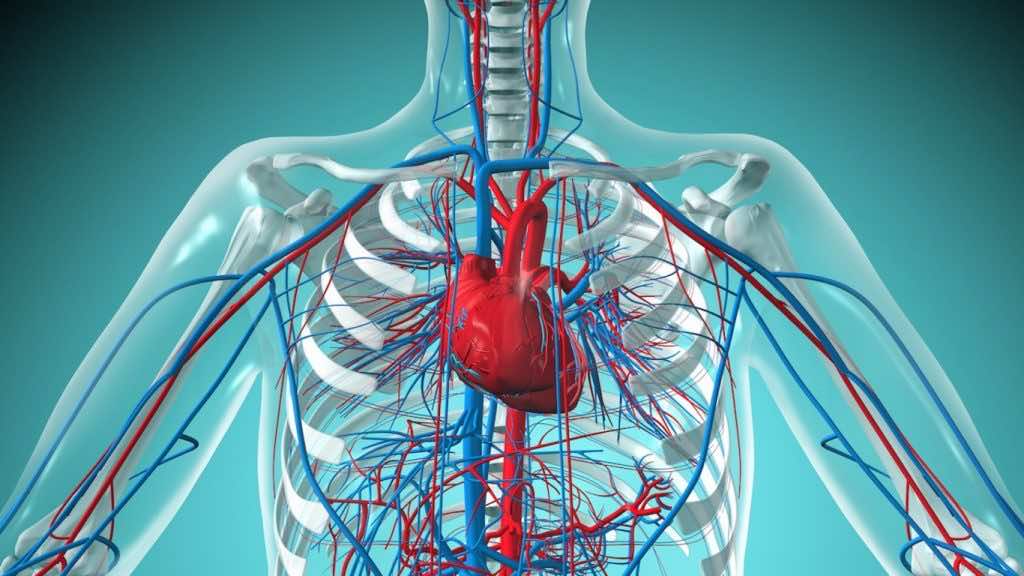
Researchers from the University of Toronto and University of Montreal in Canada have reverse-engineered a millimeter-long (0.04 inches) vessel that beats like the real heart and pumps fluid just like the muscular exit-chamber of a human embryo’s heart.
“With our model, we can measure ejection volume – how much fluid gets pushed out each time the ventricle contracts – as well as the pressure of that fluid,” says University of Toronto biomedical engineer, Sargol Okhovatian. “Both of these were nearly impossible to get with previous models.”
Joining a wave of 3D models of body parts that develop and behave just as nature intended (without unfolding into fully functional organs), this new heart-like organ was grown in a lab using a mix of synthetic and biological materials.
The cells were derived from the cardiovascular tissues of young rats, and then grown on a layer of scaffold printed out of a polymer with grooves for directing the tissue’s growth.
To turn the triple-layered stack of heart cells into something that more resembles a pulsing chamber, the team used a cone-shaped shaft they dubbed a mandrel. A quick roll in the tissue sample, and presto – a simple ventricle.
“Until now, there have only been a handful of attempts to create a truly 3D model of a ventricle, as opposed to flat sheets of heart tissue,” says senior author Milica Radisic, a chemist from the University of Toronto.
“Virtually all of those have been made with a single layer of cells. But a real heart has many layers, and the cells in each layer are oriented at different angles. When the heart beats, these layers not only contract, they also twist, a bit like how you twist a towel to wring water out of it. This enables the heart to pump more blood than it otherwise would.”
It has an internal diameter of just half a millimeter (0.02 inches) and ejects liquid at a pressure of around 5 percent of an adult’s heart.
“With these models, we can study not only cell function, but tissue function and organ function, all without the need for invasive surgery or animal experimentation,” says Radisic.
“We can also use them to screen large libraries of drug candidate molecules for positive or negative effects.”
This research was published in Advanced Biology.