UCL researchers captured the finest images of living bacteria, revealing the complicated architecture of the protective coating surrounding many bacteria and making them resistant to antibiotics.
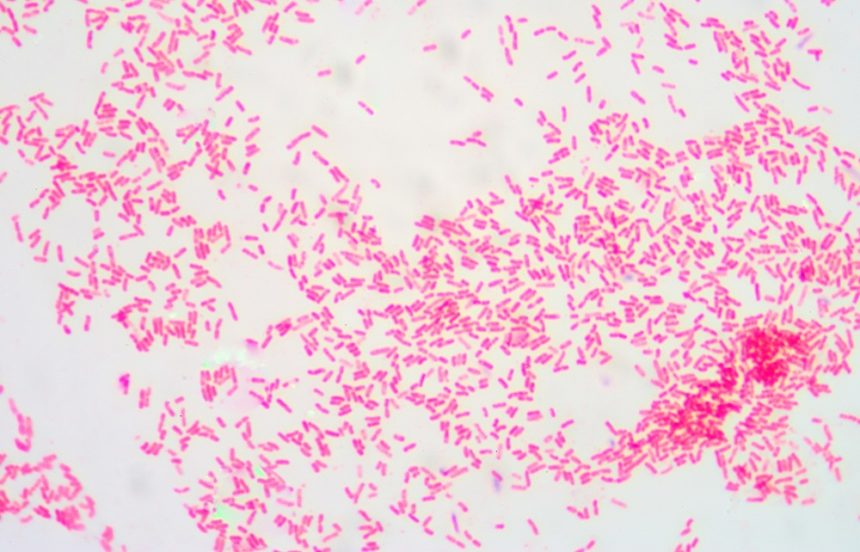
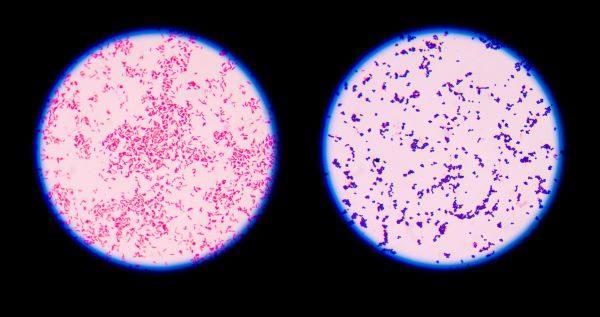
The study published in the Proceedings of the National Academy of Sciences of the United States revealed that Gram-negative bacteria, which have protective outer layers, can have stronger and weaker regions on their surface.
The bacteria’s protective outer barrier comprises dense networks of protein building blocks that alternate with protein-free patches. These patches are high in sugary chain molecules (glycolipids), which help tighten the outer membrane.
Gram-negative bacteria’s thick outer layer prevents certain medications from entering the cell, which is one of the explanations why Gram-negative bacteria’s antimicrobial resistance is seen as a greater threat than Gram-positive bacteria’s resistance, such as resistant S. aureus (aka MRSA).
“The outer membrane is a formidable barrier against antibiotics and is an important factor in making infectious bacteria resistant to medical treatment. However, it remains relatively unclear how this barrier is put together, which is why we chose to study it in such detail,” corresponding author Professor Bart Hoogenboom added.
“By studying live bacteria from the molecular to cellular scale, we can see how membrane proteins form a network that spans the entire surface of the bacteria, leaving small gaps for patches that contain no protein. This suggests that the barrier may not be equally hard to breach or stretch all over the bacterium, but may have stronger and weaker spots that can also be targeted by antibiotics.”
The researchers felt the basic architecture of living Escherichia coli (E. coli) bacteria with a microscopic needle to understand its structure. Because the needle’s tip is only a few nanometers wide, molecular structures on the bacterial surface can easily be seen.
The images show that the bacteria’s whole outer membrane is packed with microscopic pores made by proteins, allowing nutrients to pass through while restricting toxins. Despite the fact that the outer membrane contains a huge number of proteins, its packed and immovable structure caught researchers off guard.
Interestingly, the scans showed a significant number of spots that did not appear to be protein-free. Instead, these patches contain a glycolipid found on the surface of Gram-negative bacteria. The second pimple-like patch appeared when portions of the membrane were flipped inside out due to mutations. The appearance of these anomalies was linked to an increased sensitivity to bacitracin, an antibiotic effective against Gram-positive bacteria and not Gram-negative bacteria in this case.
“The textbook picture of the bacterial outer membrane shows proteins distributed over the membrane in a disordered manner, well-mixed with other building blocks of the membrane. Our images demonstrate that that is not the case, but that lipid patches are segregated from protein-rich networks just like oil separating from water, in some cases forming chinks in the armour of the bacteria. This new way of looking at the outer membrane means that we can now start exploring if and how such order matters for membrane function, integrity and resistance to antibiotics,” Georgina Benn, who performed the microscopy on the microorganisms at UCL, explained.
The findings may also shed light on how bacteria maintain a tightly packed, protective barrier while allowing for rapid growth. Under ideal conditions, E. coli doubles in size and then splits in 20 minutes. The glycolipid patches, researchers believe, allow for more membrane stretch than the protein networks, making it easier for the membrane to adjust to the bacterium’s increasing size.
The UKRI, the National Institutes of Health, the European Research Council, and the UK Department for Business, Energy, and Industrial Strategy generously sponsored the research.