A revolutionary cell therapy for asthma that can provide long-term relief with a single injection has been developed by Chinese researchers. This novel approach— an innovation based on state-of-the-art procedures commonly associated with cancer treatment— has demonstrated extraordinary efficacy in tests conducted on animals. This development lights up the horizon for millions across the globe that battle the persistent pangs of this chronic respiratory malady; an evolution to hope from despair, without having to engage in daily skirmishes against an invisible enemy.
Asthma is a global issue that affects more than 300 million people every year and causes over 250,000 deaths annually. In the United States, asthma impacts more than 27 million individuals — roughly one out of twelve Americans — as reported by the Asthma and Allergy Foundation of America. The conventional methods like inhalers or anti-body injections demand incessant lifetime intake without promising a complete recovery. But this fresh alternative treatment using CAR-T (chimeric antigen receptor T-cell) therapy pledges to revolutionize the scenario. About half of patients’ asthma is caused by specific cytokines, including as IL-4, IL-5, and IL-13, according to research conducted by Dr. Peng Min and his colleagues at Tsinghua University. Signaling proteins called cytokines are essential for regulating inflammation, but too much of them can cause serious inflammatory disorders, such as autoimmune illnesses. Although they require continuous care, the biological therapies now in use that target these proteins are successful.
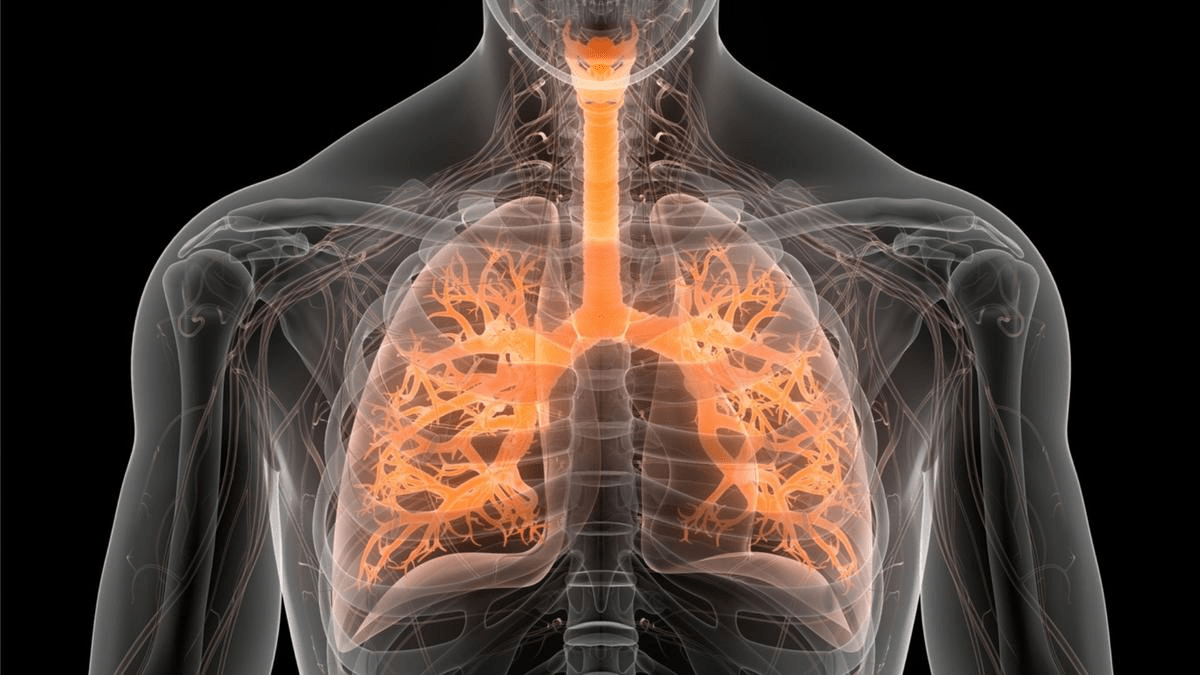
In their study, Peng’s team developed a novel method to simultaneously target these cytokines using CAR-T cell therapy. This therapy involves genetically engineering a patient’s T-cells, a type of white blood cell essential for fighting infections, to recognize and eliminate specific targets, such as cancer cells. This same principle was adapted to address asthma, resulting in remarkable outcomes. The research team found that a single infusion of these engineered cells provided sustained suppression of lung inflammation and relieved asthma symptoms for more than a year in mice.
“The new cell therapy represents an option for asthma patients to achieve long-term remission of symptoms and live a normal life with a single administration of cells,” Peng’s team reported. This development is particularly significant, as it offers a potential one-time solution for a condition that currently requires lifelong management.
The implications of this discovery extend beyond asthma. The researchers suggest that other diseases driven by similar inflammatory processes, such as allergies, atopic dermatitis, or obstructive pulmonary disease, might also be treatable with this innovative cell therapy.
Experts warn that more investigation is necessary to determine the viability and safety of this strategy in clinical settings, even in light of the encouraging results. Medical expert Bart Lambrecht of Ghent University in Belgium stressed the significance of patient selection and the discovery of biomarkers that could indicate if a therapy will be superior to current treatments. They noted that although the outcomes of the animal studies are promising, there are substantial obstacles in applying these discoveries to patients in the human race.
According to Lambrecht, “more research needs to be done on the biomarkers or clinical traits that would predict the superiority of the new CAR-T cell therapy over existing biological medical products.” This emphasizes the necessity of extensive clinical trials to guarantee the treatment’s safety and effectiveness for usage in humans.