3D printing technology is changing the world immensely, and the tech has its own perks. In our daily lives, the technology could be letting us live in houses that have been printed in 24 hours or military grenade launchers. It could be bringing us closer to green energy with printed turbine blades, or bringing comfort with luxury shoes. The technology is finding its way in health tech, and the results are exciting. A team at Northwestern University in Chicago has just 3D printed ovaries.
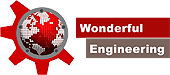
The McCormick School of Engineering and the Feinberg School of Medicine have published a collaborative study of research work in the journal Nature Communications. The team removed the ovary from a female mouse and replaced it with a 3D printed version. The mice were able to ovulate, produce healthy offsprings, and even nurse the young just like the ordinary mice moms. Reproductive scientist and the director of Women’s Health Research Institute at Feinberg, Teresa Woodruff said:
“This research shows these bioprosthetic ovaries have long-term, durable function. Using bioengineering, instead of transplanting from a cadaver, to create organ structures that function and restore the health of that tissue for that person is the holy grail of bioengineering for regenerative medicine.”
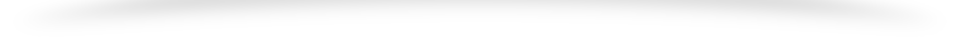
The team developed a gelatin made from broken-down collagen to be used as the ink for the printer. The aim was to create an organic ink that was strong enough to stay intact during surgery. The collagens used for making the ink are safe to be used by humans as well. Usual hydrogels are too weak to retain their structure, but this gelatin was different. An assistant professor of materials science and engineering at McCormick commented, “No one else has been able to print gelatin with such well-defined and self-supported geometry.”
The team first determined the structure of natural mice ovaries and used it as a skeleton to develop the implant. The scaffold they created had pores that can help the eggs get wedged in the structure thus boosting their survival and stimulating hormone production.

The success of the technology in mice has raised the expectation of the same being used in humans. The aim of the research is to restore fertility in women undergoing cancer treatments whether as adults or as children. One of the lead authors of the study Monica Laronda explained, “What happens with some of our cancer patients is that their ovaries don’t function at a high enough level and they need to use hormone replacement therapies in order to trigger puberty. The purpose of this scaffold is to recapitulate how an ovary would function. We’re thinking big picture, meaning every stage of the girl’s life, so puberty through adulthood to a natural menopause.”

Researchers have already developed an artificial womb that could help premature babies grow normally, and this development seems to be a further improvement for the people struggling with bringing a child of their own in the world.